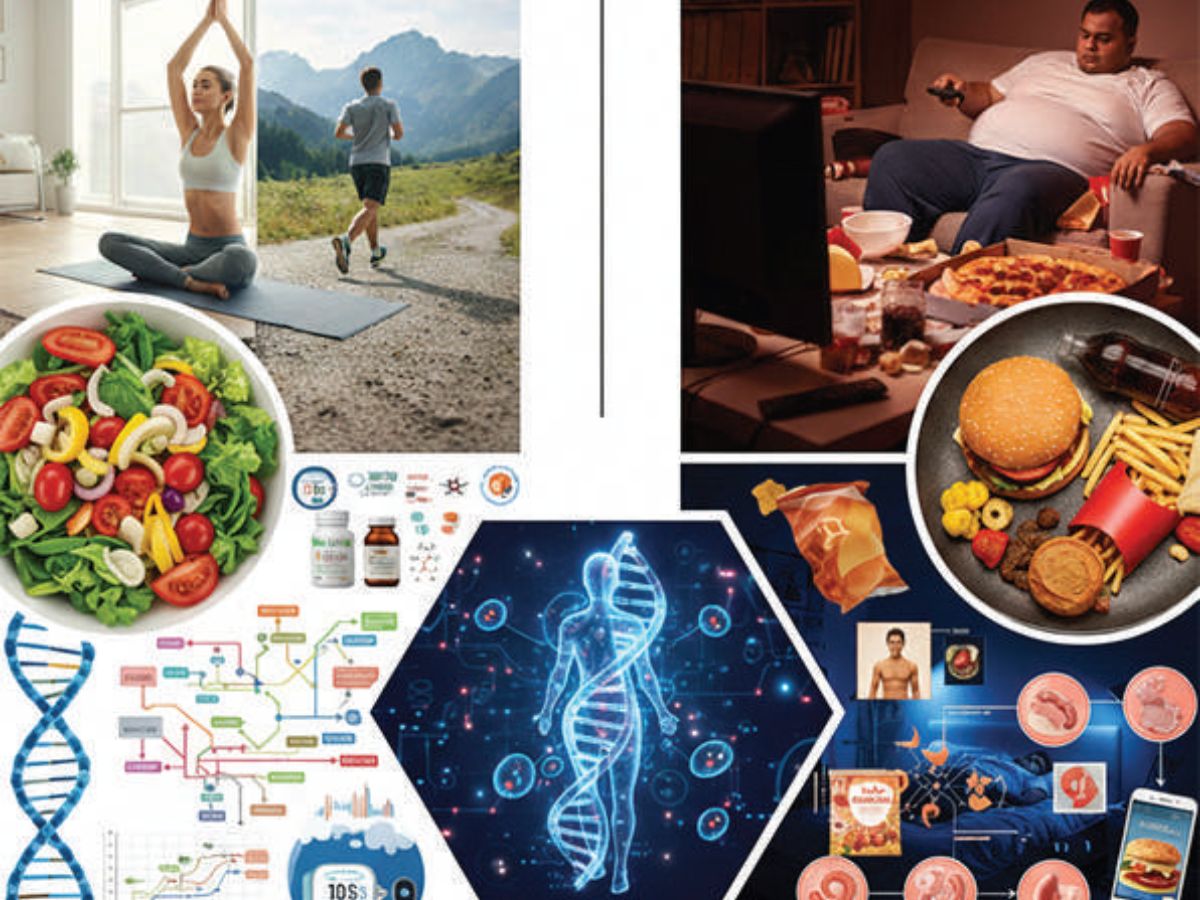
Many misconceptions lead to body shaming of the Obese and the Skinny by ridiculing or mocking them, and further damage the self-esteem of the victim. Misconceptions about the obese are that they lack self-control and willpower to change, are irresponsible, gluttonous, and lazy. In reality, obesity is a complex medical condition influenced by genetics, environment, hormones, mental health, and socioeconomic factors, not just personal choices. Obese individuals can be active and healthy despite their weight. Many believe obesity is a cosmetic issue and that only severe cases need medical attention, even though it is a serious disease with silent health risks like heart disease, diabetes, and sleep apnoea (breathing blockage), and even a small weight loss offers significant benefits.
The main misconception about skinny people is that they eat less and are trying to fit unhealthy societal beauty and fitness standards. Even lean and fit people are often perceived as unhealthy. On the other hand, a person perceived as a health icon may have a major undiagnosed health risk. A fat person on a healthy, balanced diet and active lifestyle is healthier than a thin person with a sedentary lifestyle, consuming ultra-processed fast foods.
WHY SOME ARE WARM WHILE OTHERS FEEL COLD
Heat production depends on the metabolic rate and is influenced by factors like thyroid hormones, sympathetic stimulation, and physical activity. Heat generation varies significantly depending on the body’s activity level, like muscle contraction, and high biochemical activity, as in the liver, generates much more heat per mole of oxygen used than heat generated by basal functions (obligatory thermogenesis). Involuntary muscle contractions (shivering) can more than double metabolic heat production to combat cold.
WHY SOME GAIN EXCESS BODY FAT WHILE OTHERS DO NOT
Metabolism differences, caloric imbalances, hormonal disturbances, genetic and epigenetic variations, appetite alterations, and lifestyle and environmental factors all influence the body fat and muscle content, and the biological differences between underweight, ideal weight, and overweight individuals. Skinniness or being underweight is caused by a combination of high metabolism, genetics, inadequate calorie intake (inability to chew/swallow food, chronic starvation, eating disorders), and underlying physical or mental health conditions. Other factors include hyperthyroidism, digestive disorders like Celiac Disease (gluten intolerance) and Inflammatory Bowel Disease (Crohn’s Disease, Ulcerative Colitis), chronic infections like Tb and HIV/AIDS, cancer, or stress causing loss of appetite.
CALORIE INTAKE–OUTPUT MISMATCH
Weight gain occurs when caloric intake consistently exceeds energy expenditure. Excess calorie intake stems from:
- Behavioural habits: mindless eating, large portions, high-fat foods, and sugary drinks while distracted (TV, phone),
- Environmental factors: easy access to cheap, processed food,
- Psychological triggers: stress, boredom, emotional eating,
- Hormonal disruption: Sleep deprivation disrupts appetite-controlling hormones.
- The social influence of family and friends’ eating habits of larger portions, calorie-rich snacks, sugary drinks, and alcohol.
- The brain takes about 20 minutes to get fullness signals; rapid eating drives overconsumption.
- Lifestyle choices: sedentary jobs, lack of physical activity.
METABOLIC DIFFERENCES
- Central obesity leads to hypertension, dyslipidaemia, impaired glucose tolerance, and chronic inflammation (Metabolic Syndrome).
Individuals with higher metabolism or greater non-exercise activity thermogenesis (NEAT), like fidgeting or restlessness, or a very active lifestyle, or overactive thyroid (hyperthyroidism), burn more calories, and are likely to remain lean or underweight. The obese have a higher metabolic rate to maintain the greater body weight, but their metabolism is inefficient (insulin resistance and impaired fat oxidation) due to excess fat and less muscle mass. - Individuals with lower basal metabolic rate (BMR), like those with underactive thyroid (hypothyroidism), excess cortisol (Cushing’s Syndrome), insulin resistance as in Polycystic Ovary Syndrome (PCOS), or lower muscle mass, burn fewer calories and gain weight even if they eat less.
- Certain medications like antipsychotics, certain antidepressants, beta-blockers, and steroids lower the metabolic rate, increase fat storage, and boost appetite, leading to weight gain.
- Excess visceral fat (fat around organs), high alcohol, caffeine, and sugar consumption, stress, and poor sleep raise cortisol in combination with high insulin levels, increasing visceral fat.
THE HUNGER PANGS: FACTORS INCREASING APPETITE
- Stress: Under stress, the release of cortisol hormone disrupts normal appetite signals, increases hunger, and triggers cravings for high-calorie, sugary, and fatty “comfort foods”.
- Anxiety disorders: Anxiety also elevates cortisol levels, increasing the frequency of hunger pangs for high-fat, high-sugar foods.
- Emotional response: Extreme hunger can be a response to cope with stress, boredom, anxiety, or depression.
- Hormones: Hunger hormone leptin signals fullness (satiety) and ghrelin signals hunger. Poor sleep, intense exercise, and fasting decrease leptin and increase ghrelin and appetite. Excess body fat causes high leptin levels that the brain ignores (leptin resistance) and reduced suppression of the “hunger hormone” ghrelin. This creates a vicious cycle where the body falsely signals starvation, promoting overeating.
- Non-esterified fatty acids (NEFAs): Elevated levels of NEFAs in obese individuals mislead the brain into thinking that the body is in a state of starvation, promoting overeating.
- Inflammation: Chronic, low-grade inflammation associated with excess body fat reduces the brain’s (hypothalamus) hunger sensitivity to satiety signals.
- Blood Sugar Fluctuations: Refined carbs cause a steep rise, followed by a low blood sugar that triggers intense cravings for repeated frequent consumption of refined carbs.
- Altered brain reward pathways: High-calorie foods can rewire the brain’s pleasure centres, similar to addiction, increasing cravings regardless of physical energy needs.
- Genes: Certain FTO (fat mass and obesity-associated) gene variants increase appetite. Mutations in the MC4R (satiety-regulating) gene increase appetite. LEPR gene variations can affect leptin hormone efficacy.
EPIGENETIC AND GENETIC DIFFERENCES
Epigenetic changes are modifications to DNA or its associated proteins (histones) that switch a gene “on” or “off”, without changing the actual DNA sequence, and can be influenced by environment (diet, stress, pollutants, smoking, drug abuse, exercise), and age. These changes can be stable, and even inherited across generations, linking the environment and age of parents and ancestors to the long-term health and disease (cancer, diabetes, heart disease, and neurodegenerative disorders) risk in the family. Genetics influence appetite regulation, fat distribution, and storage. Some individuals have a genetic predisposition to store fat, while others possess a genetically higher basal metabolic rate and burn more calories at rest. Multiple genes with small effects collectively determine the genetic susceptibility to obesity or skinny build. PPARG (master regulator), ADRB3 (receptor on fat cells), UCP1 (protein in brown fat), and PRDM16 (master transcriptional regulator) are key regulatory genes and proteins involved in adipogenesis (the formation of fat cells), specifically in the development and function of brown adipose tissue (BAT) and the “browning” of white adipose tissue (WAT). They are critical for thermogenesis (heat production) and energy metabolism, often acting in concert to combat obesity and improve insulin sensitivity. Genetic predispositions, such as those associated with celiac disease (HLA genes), can cause inflammation in the gut wall, leading to severe malabsorption and weight loss.
TESTS AND LIFESTYLE CHANGES TO IMPROVE METABOLISM
- Body fat mass and lean mass (Body weight – fat mass) can be accurately measured by Dual-energy X-ray absorptiometry (DEXA), hydrostatic weighing, or Air Displacement Plethysmography (Bod Pod). Common, accessible, and less precise methods include bioelectrical impedance analysis (BIA) scales and skinfold callipers. BMI and Waist-hip-ratio have been explained in an earlier article. Infrared thermography helps assess Brown Adipose Tissue (BAT).
- Biochemical tests include HbA1c, lipid profile (explained last Sunday), thyroid and liver function tests, insulin and HOMA-IR (Fasting Insulin x Fasting Glucose / 22.5), and inflammatory markers CRP and IL-6.
- Nutrigenetic tests analyse genetic variations that influence the body’s response to nutrients and help personalize nutrition advice.
- Insulin sensitizing through lifestyle changes (diet, exercise, sleep, and stress management) is key to improving metabolic function.
- Strength training to build lean muscle mass helps increase the resting metabolic rate.A fibre-rich low-calorie diet can improve body composition and metabolic health.
Stigma prevents the obese and skinny from seeking necessary care. They need to be motivated, not ridiculed. The skinny may have serious health issues. The obese have serious risks like heart disease, diabetes, and sleep apnoea. Parents should not assume that obese children will “grow out of it”. While genes play a role, lifestyle and environment contribute significantly. Bariatric surgery and weight loss drugs are not cosmetic; they are necessary for severe obesity, though they do have major consequences and side effects.
-
Dr P.S. Venkatesh Rao is a Consultant Surgeon, Former Faculty CMC (Vellore), AIIMS (New Delhi), and a polymath in Bengaluru, drpsvrao.com