CHOLESTEROL: THE GOOD, THE NOT SO BAD, AND THE UGLY
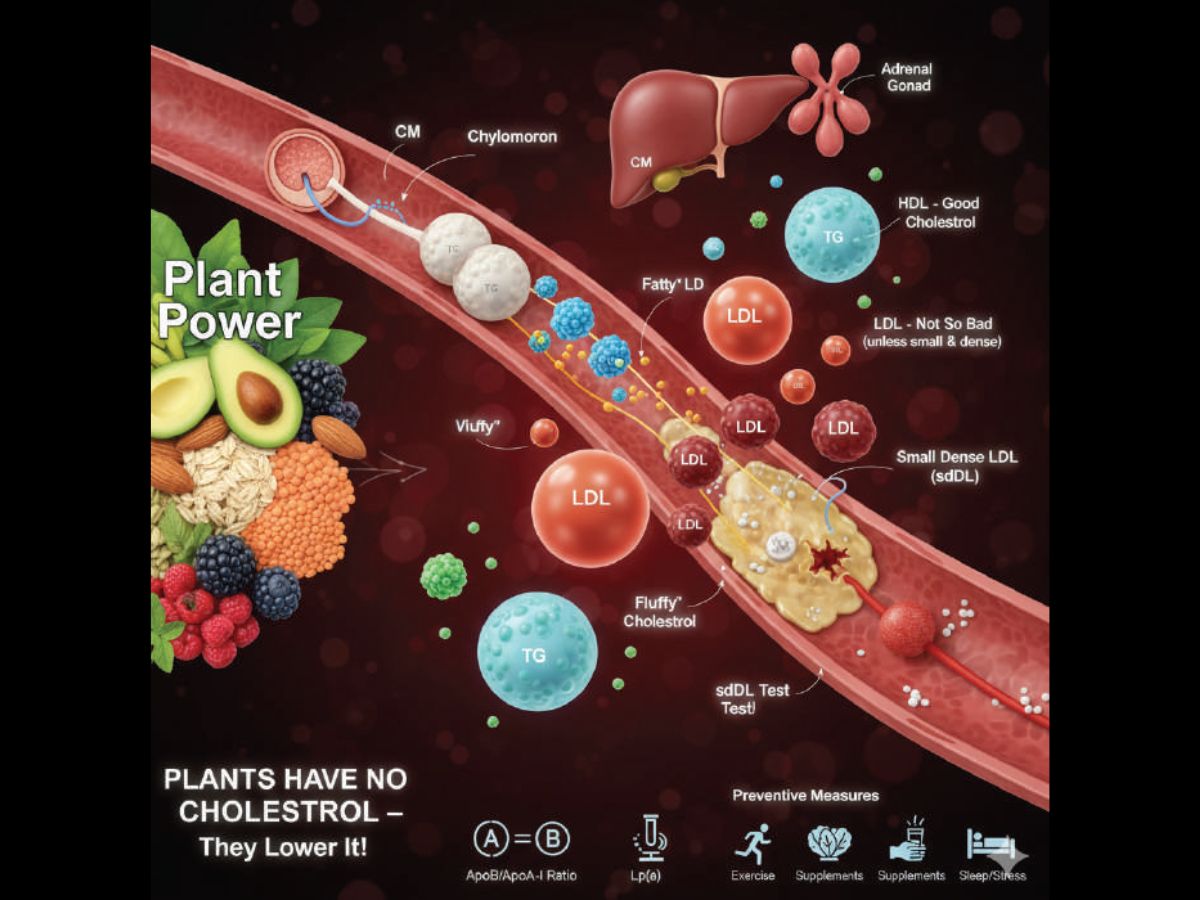
Cholesterol is a waxy substance essential for healthy cell membranes, and hormone production, particularly steroid hormones like oestrogen, testosterone, and cortisol. Excess cholesterol is converted into bile acids in the liver, which act as soapy emulsifiers necessary for the digestion, absorption, and transport of fats, fat-soluble vitamins (A, D, E, K), and nutrients. All our cholesterol is produced by our liver or is from animal foods (meat, poultry, dairy products). As fats like cholesterol and triglycerides do not mix with water-based blood, they are carried by complex, spherical particles called Lipoproteins engineered to transport water-insoluble lipids (fats) through the bloodstream.
LIPOPROTEINS: Lipoproteins consist of a core of fat (triglycerides and cholesterol esters) to be transported, surrounded by a shell of phospholipids, unesterified (free) cholesterol, and special proteins called apolipoproteins, that enable this complex assembly to be fully miscible and transportable in the blood. They are classified in increasing size and decreasing density as HDL (High-Density Lipoprotein), LDL (Low-Density Lipoprotein), IDL (Intermediate-Density Lipoprotein), VLDL (Very-Low-Density Lipoprotein), and chylomicrons (CM). Cholesterol is mainly carried by LDL from the liver through the arteries, and returned by HDL to certain endocrine organs and the liver. VLDL carries triglycerides. IDLs are the remnants of VLDL. Chylomicrons are lipoproteins formed in the gut (intestines) after a meal to transport dietary fats (triglycerides, cholesterol) to tissues like muscle and fat for energy or storage. They are too large to directly enter the bloodstream and enter it via the lymphatic system.
HDL, THE GOOD CHOLESTEROL: It is the densest lipoprotein because it contains the highest proportion of protein to lipids. HDL carries cholesterol, phospholipids, and triglycerides from all parts of the body to steroid hormone-producing (steroidogenic) endocrine organs such as the adrenals, ovary, and testes, and excess back to the liver for excretion in bile or re-use. HDL particles enlarge while circulating in the blood, aggregating more fat molecules and transporting up to hundreds of fat molecules per particle. HDL is called the “good cholesterol” because it removes cholesterol and fats from cells, including within the artery wall atheroma, reduces macrophage accumulation, and thus helps prevent or even regress atherosclerosis. Those with HDL levels less than 40 mg/dL (or about 1 mmol/L) have increased rates of heart disease. However, a higher than 50 mg/dL blood level of HDL is not necessarily protective. Extremely high levels indicate increased cardiovascular risk, especially in hypertensive patients. HDL levels can be raised with a high fibre diet, exercise, weight (body fat) reduction, omega-3 fatty acids, niacin, and magnesium supplements, and avoiding smoking, alcohol, sugars, refined carbs, saturated and trans fats.
LDL, THE NOT SO BAD CHOLESTEROL: LDL is now further differentiated into “fluffy” (large, buoyant) and “compact” small, dense LDL (sdLDL) particles. LDL is essential for the transport of cholesterol, and is “bad” only if its smaller, denser type is in excess. Cholesterol-carrying sdLDL is more capable of penetrating the artery walls than the large LDL. This leads to atheromatous plaque (or atheroma) formation, a sticky, fatty, soft deposit in the inner lining of arteries, composed of cholesterol, fats, calcium, and other substances. This process, called atherosclerosis, hardens and narrows arteries, restricting blood flow to various parts of the body. Sudden plaque ruptures lead to clots that block blood flow, causing heart attacks, strokes, and affecting other vital organs and parts of the body. LDL-C (Cholesterol) measures the amount of cholesterol, and LDL-P (Particle) measures the number of LDL particles. Optimal LDL-C level is presently considered less than 100 mg/dL; levels above 160 mg/dL are considered high; and levels above 190 mg/dL are considered very high. For those with existing heart disease or at high risk, the target is lower than 70 mg/dL. LDL-C levels can be lowered by a diet rich in fibre, healthy fats, and plant sterols, avoiding saturated/trans fats, regular exercise, maintaining a healthy weight, quitting smoking and alcohol, managing stress, and getting enough sleep. Statins are prescribed if these changes aren’t enough.
TRIGLYCERIDES (TGs): Excess calories from foods rich in fats, oils, and carbs consumed are converted into triglycerides and stored in fat cells as an energy reserve. TGs, while essential at normal levels below 150 mg/dL (milligrams per decilitre), at high (above 200 mg/dL), or very high (above 500 mg/dL) levels, especially with low HDL or high LDL cholesterol, can promote atheroma formation and increase the risk of heart disease, stroke, and even pancreatitis. High TGs are often a sign of obesity, metabolic syndrome, poorly managed diabetes, and hypothyroidism, and are linked to calorie-rich, unhealthy diets and inactivity. They can usually be managed with lifestyle changes like low calorie diet (avoid sugars, refined carbs, saturated/trans fats, and alcohol), exercise, and weight management.
THE UGLY AVOIDABLE CONTROVERSIES: The statin versus anti-statin lobby arguments in the media sometimes turn ugly when statins and their usage guidelines are aggressively promoted, and the anti‑statin lobby vociferously objects to statins as over‑prescribed, with under‑reported side effects. This creates doubts and fears among patients, who stop medication, and ignore risk factors and symptoms till it is too late.
LIPID PROFILE TEST: It measures HDL, Non-HDL atherogenic lipoproteins, LDL-C, VLDL, IDL, and Triglycerides levels, and requires 12 hours of fasting. A better measure of heart disease risk for those with diabetes or high triglycerides is an advanced panel for LDL-P. An even more specific measure is the “Small Dense LDL” test for the highly atherogenic subfraction of LDL-P. It is more expensive and not widely available (only the Thyrocare lab does it in India).
APOLIPOPROTEIN A & B: ApoA (specifically ApoAI) and ApoB are key proteins in lipid transport, with ApoA-I being the main component of HDL, while ApoB is the sole protein in atherogenic particles LDL, VLDL, and IDL, each of which contains one ApoB molecule, making ApoB a better marker for the number of harmful particles than LDL-C or LDL-P. ApoB/ApoA-I ratio is a superior predictor of cardiovascular events (heart attack, stroke) compared to LDL /HDL ratio. Measuring ApoA-I and ApoB levels doesn’t require fasting.
LIPOPROTEIN(a) (Lp(a)): It is a genetically inherited particle in the blood that carries cholesterol, similar to LDL, but increases cardiovascular risk, and affects about 1 in 5 people. Because it is genetic, lifestyle changes don’t significantly lower it, making this simple, nonfasting blood test important to assess risk, especially with a family history of early heart disease. Levels above 30-50 mg/dL are considered an increased risk even in otherwise healthy individuals. Management includes lowering other risk factors like LDL and blood pressure, and the use of new therapies targeting Lp(a).
PLANTS DO NOT HAVE CHOLESTEROL: Plant sources like coconut and avocado have healthy fats and beneficial plant sterols, but do not contain cholesterol, which is uniquely of animal origin, produced by the liver of animals and humans. Plants synthesize their own versions of these molecules, called phytosterols. These phytosterols are structurally similar to cholesterol but are beneficial to human health because they compete with cholesterol for absorption in the digestive system, and lower blood cholesterol levels. High-fibre foods bind bile salts and cholesterol, reducing absorption of dietary cholesterol. Nuts (almonds, walnuts, peanuts), seeds, whole grains (oats, wheat germ, brown rice), legumes (beans, lentils), fruits (avocado, berries, citrus), and vegetables (carrots) are rich in sterols and can help reduce cholesterol absorption in the gut.
TESTS AND PREVENTIVE MEASURES FOR “HEALTHY” PERSONS: It is essential to test for Lp(a) and ApoB, more than a basic lipid profile panel. The sdLDL (small dense LDL) test is a more specific measure of risk than LDL, but not widely available. Elevated Highly Sensitive C‑reactive protein (HS-CRP) an inflammatory marker, and elevated Homocysteine are associated with increased cardiovascular risk. Correct high ApoB, sdLDL (or LDL), triglyceride levels, and low HDL levels by diet, exercise, lifestyle changes, medication, and supplements, as already mentioned, and by controlling diabetes and obesity to reduce cardiac, stroke, and other atheroma risks.
Dr. P.S.Venkatesh Rao is a Consultant Surgeon, Former Faculty CMC (Vellore), AIIMS (New Delhi), and a polymath in Bengaluru, drpsvrao.com